

Written by Dr Miriam Stoppard OBE
Dr Miriam Stoppard has spent many years as a TV doctor including having her own show for 15 years — as well as authoring over 80 books and writing columns for the Daily Mirror.
Around 10 million people in the UK have arthritis, or similar conditions that affect the joints. Stannah’s Health and Wellbeing Advisor, Dr Miriam gives her advice on living with the two most commons types of arthritis: osteoarthritis and rheumatoid arthritis. In part one, Dr Miriam introduces us to osteoarthritis.
Introduction
What is arthritis?
Arthritis, literally an inflammation of the joints, includes a group of conditions that cause stiffness, swelling and pain in the joints. Arthritis sometimes co-exists with skin diseases such as psoriasis, intestinal disorders such as Crohn’s disease and autoimmune diseases such as lupus.
There are several different types of arthritis, each being distinctive, each requiring its own treatment and management. The most common is osteoarthritis (OA), usually affecting middle-aged and older people in the weight bearing joints - the knees and hips. After the menopause it can affect the ends of the fingers. Spondylosis is a common form of osteoarthritis that affects the joints in the spine, mainly the neck (cervical) and lower back (lumbar) regions.
What is osteoarthritis?
There’s gradual degeneration of the cartilage covering the ends of bone inside joints which, due to wear and tear over many years, causes the pain, swelling and stiffness of osteoarthritis.
The condition, affecting 8.5 million people in the UK, rarely appears before middle age and primarily affects the weight-bearing joints – the hips and knees. Around the age of the menopause, the terminal joints of the fingers show osteoarthritic change with the appearance of bony outgrowths on the side of the joints – Heberden’s nodes. Any joint that’s injured could become osteoarthritic at a later date. The greater the wear and tear in early life, the greater the chance of osteoarthritis (OA) setting in. OA is almost always asymmetrical.
Most people over the age of 60 have some degree of OA and three times as many women are affected as men. The areas most commonly affected are the large spinal joints of the lower back, hips, knees, ankles and feet. A thickening of the bone ends causes bony spurs to appear at the edge of joints.
Exactly the same process occurs at the edge of the neck (cervical) vertebrae, often causing a stiff neck that makes movement painful. This condition is known as cervical spondylitis.
What are the symptoms of OA?
As well as pain, OA also causes swelling, creaking and stiffness of the affected joints. The pain is frequently worse at night after a day of wear and tear. Pain is also worsened when the body heats up in bed at night as all inflamed tissues swell.
- Weakness and shrinkage of surrounding muscles may occur if pain prevents the joint being used regularly.
- Pressure from a bony spur on a nerve in the neck (cervical spondylitis) may cause pain in the shoulder, elbow and fingers.
- When bony growths occur in the lower back (lumbar spondylitis), pressure on the sciatic nerve will cause pain in the buttock and the back of the legs down to the sole of the foot, pain known as sciatica.
How’s it diagnosed?
The crucial picture is classical of OA and confirmation is with X-ray findings.
What’s the treatment?
Unfortunately, there’s no cure although the symptoms can be relieved by painkillers and non-steroidal anti-inflammatory drugs, NSAIDs (read part two of this blog here ).
- Physiotherapy, heat treatment and exercise are helpful for pain relief and mobility.
- Corticosteroid injections can sometimes bring instant, if temporary, relief but must be used sparingly.
- Joint replacement can restore mobility to a severely affected joint, mainly hip and knee.
Exercises for people with osteoarthritis
- Hold your arms straight down but across your body, then lift them upwards and outwards, uncrossing them as you go. With your arms in this position, clasp your hands behind your head.
- Push your toes and feet down and then pull them up towards you. Move your toes and ankles around in a large circle.
- Lie down, preferably on the floor, bend each leg in turn up onto your chest towards the opposite shoulder.
- Rest your arms on the table or arm of a chair without supporting your hand. Bend your hand down towards the floor and then lift it up. Next, move you hand to the left and then to the right. When you’re doing this make sure your hand rests in the mid-position and is in line with your forearm and doesn’t fall forwards.
- Bend your fingers and grip tightly, then stretch and spread your fingers. Touch the tip of each finger in turn with the thumb.
If sitting in a cramped seat becomes painful after half an hour or so, stand up and walk around or massage your knees. Don’t sit with your legs crossed – it isn’t good for the knees.
As with any type of arthritis, exercise must always be balanced with rest, so don’t overtire your affected joints and be careful not to overstretch them while resting.
For further information, continue reading Miriam's Part Two where she discusses Rheumatoid Arthritis - click here to learn more.
Stay up to date
Latest Blogs

Whole Home Comfort with Stannah and HSL

Dame Zandra Rhodes x Stannah: When accessibility meets style
Could more people benefit from home adaptation support for hidden disabilities?
50 years of Stannah Stairlifts – A milestone grounded in purpose

BBC’s Dr Punam Krishan reveals a little-known Parkinson’s symptom to watch for...
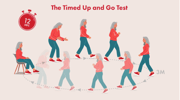
Are you at risk of falling? Dr. Punam Krishan’s simple 12-second test could tell you...
Snore Wars: Could sleeping separately be the secret to a better night’s rest?

Proud to carry the Made in Britain mark!
Stairlifts made for you
All our stairlifts whether straight or curved are customised to suit you and your home so call now to arrange a visit to get your FREE personalised quote!